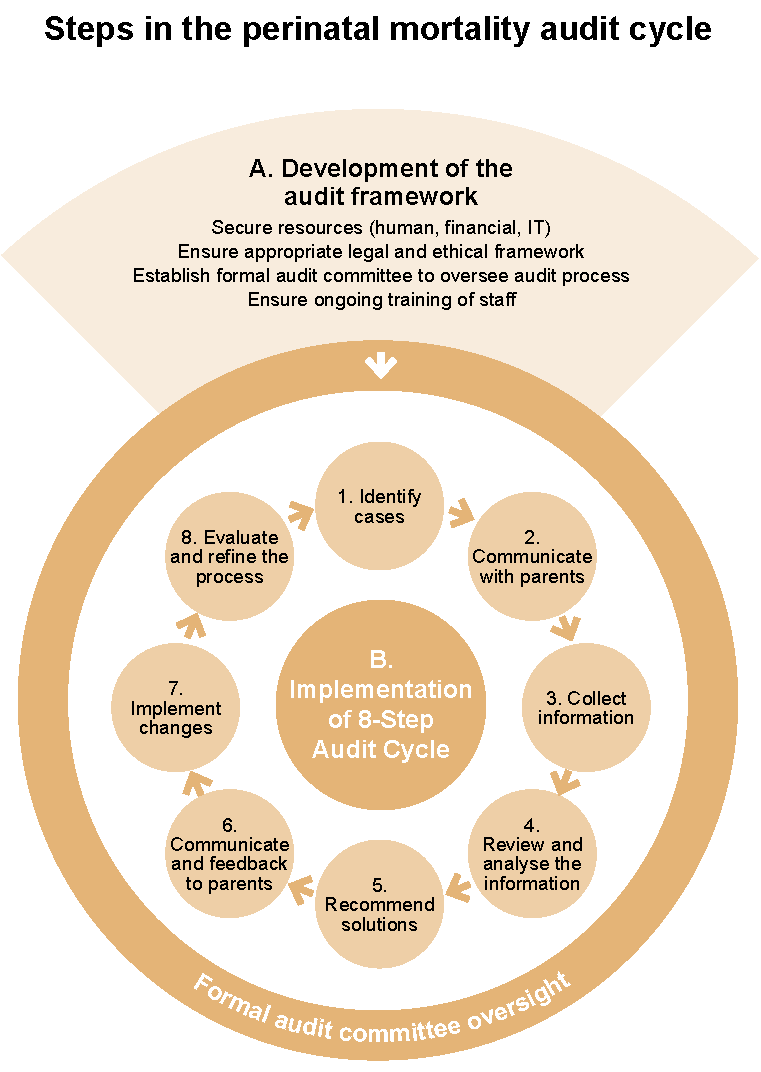
The WHO Making every baby count: Audit and review of stillbirths and neonatal deaths guideline recommends that following a perinatal death, a systematic review of the causes and circumstances leading up to and surrounding that death take place within the hospital service.2 The six-step cycle from the WHO guideline2 with an additional two steps to engage with and provide feedback to parents32-34 is suggested (Figure 1). An audit framework (Part A) underpins the eight steps of the audit cycle (Part B) and must be established before the audit cycle can be implemented.
Evidence-based recommendation 7.1
Evidence quality: Moderate confidence
All maternal and newborn services should implement a formal process for perinatal mortality audit, including identification of causes, associated conditions, and contributing factors relating to care.
Consensus-based recommendation 7.2
Smaller services, including those in rural and remote regions, are encouraged to participate in combined perinatal audit meetings with other experienced maternal and newborn services to ensure high-quality audit.
Consensus-based recommendation 7.3
If a baby dies outside the hospital of birth, the audit should ideally be carried out by the hospital where the baby was born. Communication between hospitals that provided care is needed to ensure the perinatal mortality audit committee has access to all relevant details.
Healthcare professionals may be reluctant to participate in perinatal audit meetings because of high workload, lack of communication and education regarding perinatal mortality audit meetings, fear of blame, fear of litigation, and failure to implement change.3,4,35 A standing multidisciplinary perinatal mortality audit committee and a permanent chairperson role to oversee each perinatal mortality audit meeting can increase attendance and improve the impact of audit outcomes in policy review and improvements.3,31 Ideally, the perinatal mortality audit committee should include key stakeholders who reflect all areas of the healthcare system caring for women, babies, and their families/whānau to drive improvements across a range of specialties.36,37 Members may be representatives from neonatology/paediatrics, obstetrics, midwifery/nursing, pathology, clinical genetics, pharmacy, epidemiology/statistics, social work, general practice, and administration.2,38 Studies consistently recommend standardised training for healthcare professionals to ensure high quality data on causes of and factors contributing to perinatal deaths4,39 and to support communication with parents during the audit process.34,40
The hospital administration should establish a standing multidisciplinary perinatal mortality audit committee and should support the committee through:
Consensus-based recommendation 7.4
All maternal and newborn services should ensure that appropriate systems for undertaking perinatal mortality audit, reporting of findings, and implementation of recommendations are in place and that the perinatal mortality audit committee is adequately supported to ensure perinatal mortality audit is conducted effectively.
Level 3, Aubigny Place
Mater Research Institute
Raymond Terrace,
South Brisbane QLD 4101
The University of Queensland Faculty of Medicine
